I see a resuscitation like Tom Brady and the Patriots playing a game on their way to the Super Bowl.
Yes, they have a good leader, in fact, the best quarterback of history, and they also have other good individuals. But more importantly, they are winning AS A TEAM. They trained, rehearsed, planned everything. And then they did it again.
You have all experienced different communication style in the resuscitation room and we all know we can do better. After reading a bunch of stuff this summer, I have decided to make a summary and share it with you.
Communication is the kind of things that we generally think we are ok at, if you would ask anybody. But the fly on the wall would tell us there is generally room for improvement. Myself included, of course.
Tom Brady might well be the best quarter back of his generation, but the Patriots could not have win six Super Bowls if he only showed to the game and not to practices.
Can you play ball if you don’t come to practices?
Below are some communication strategies that need to be practiced and practiced again. This is why it is crucial to do regular drills and simulations to reinforce it, and that are members of the team be present.
Here are the key points to be a good leader :
- Start with the Zero Point Survey, using the STEP-UP strategy
- Use closed-loop communications
- Share your mental model with your team. Tell them where we are at, where we are going
Closed-loop communication
Closed-loop communication (CLC) involves three steps: (1) the sender transmits a message: the CO (call-out), (2) the receiver accepts the message and acknowledges its receipt, the check-back and (3) the sender verifies that the message has been received and interpreted correctly (ie, the loop is closed ” (Härgestam and al.)
Again :
- Sender initiates the message.
- Receiver accepts the message and provides feedback.
- Sender double-checks to ensure that the message was received and closes the loop.
Example:
Hallgrímur : Svanbjört, when you go to the store, I want you to get me two bottles of Lýsi.
Svanbjört : You want me to get you 2 bottles of Lýsi when I go to the store?
Hallgrímur : Yes.
In the resuscitation room, that would go more like this :
Leading Doctor: Freyja, I want you to give the patient 75mg of S-Ketamine then 100mg of Rocuronium. Tell me when it is given.
Freyja (Nurse): I will give 75mg of S-Ketamine then 100mg of Rocuronium to the patient then tell you when it is done.
Doctor: Correct.
Nurse : S-Ketamine and Rocuronium given.
Leading doctor: Now, I will intubate the patient.
Here is a mish-mash of evidence :
Closed-Loop = Associated with higher-performing team
“Teams that described in clear terms the emergency (CO) and used feedback (CLC) were more efficient in completing critical tasks (administering Mg infusion during an eclamptic event) than teams that were ambiguous in their communication” (Härgestam and al.)
Closed-loop = Faster care
” There was a significant reduction in time-to-task-completion when closed-loop communication was utilized (p < 0.0001). Orders with closed-loop communication were completed 3.6 times sooner as compared to orders with an open-loop [HR = 3.6 (95% CI: 2.5, 5.3)]. » (El-Shafy and al.)
Zero point survey
Zero Point Survey is just brilliant. The main idea is that a resuscitation starts even before the patient has rolled in the department. Most of the time, we receive the heads up from the prehospital crew so we can prepare our team.
Zero Point Survey, in summary : « In an organized resuscitation the primary survey must be preceded by a series of steps to optimize safety and performance and set the stage for the execution of expert team behavior. Even in the most time critical situations, an effective team will optimize the environment, perform self-assessments of personal readiness and participate in a preemptive team brief. » (Reid and al.)
STEP-UP
Self : control your own physiological response to stress (Breathe-Talk-See-Focus)
Team : get your team prepared and equipment ready
Environment : light, noise, space, control overcrowding (we don’t need 10 doctors at the bedside)
Patient : primary survey (ABCDE, C-A-B, etc. )
Update : periodically update your team
Priorities : establish team priorities (i.e. CT vs surgery first, intubation, chest tube, etc)
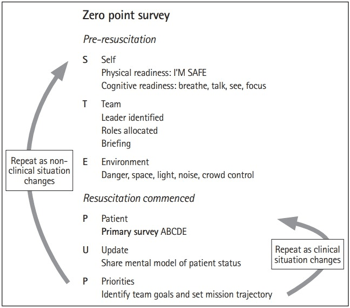
***If you are looking for a 10 minutes movie that will pump you to get better and have better team dynamics and communications, this one is for you : https://emcrit.org/emcrit/emcrit-wee-zero-point-survey-video-by-cliff-reid/
Shared mental model
This goes in the line of the STEP-UP model, particularly the update on the patient status and the priorities.
Basically, frequent and concise updates make sure that what is going in your head is well understood by the team. For example, in a case, it might be clear to you that a patient needs to be intubated, but it might not obvious to another person, so you have to relay the information.
We should do a small update with the team about every 5 minutes.
Example :
Team leader : « Alright team, just to summarize, we have a young adult male who came after a motor bike accident. He has a suspected head trauma with decreased LOC and no other identifed major injuries. We need to prepare for intubation and also we need to call the CT for imaging and we need to call the neurosurgery team.
Shared-mental model = improve patient care
In video-filmed trauma simulations, having a leader that pushes information to the team and makes updates is correlated with improved patient care. Pushing information means that the team leader is now waiting to be asked for something, but he will share, or push, the information to the team by himself.
« a positive correlation between leaders sharing information without an explicit demand for the information (“push” of information) and quality of medical management »
« these results follow the theory of SMM, in which teams with the best SMM can coordinate, communicate, and eventually perform better than teams with a less sophisticated understanding of the actual situation the team faces. Research has accumulated substantial support for the general presumption that SMMs are associated with better team effectiveness » (Johnsen and al.)
Shared-mental model = useD by efficient team
« From a series of studies conducted on military tactical teams, it has been reported that effective team performance under a high workload is dependent on the team members’ ability to apply a shared understanding of the task, the structure of the team, and the team members’ roles within it. » (Westli and al.)
Translation : when all the team members know what is going on and where they are heading, the team performs better. Please share your mental model with your team.
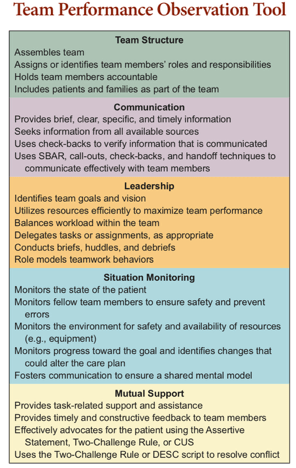
Team STEPPS
To go somewhere, it is good to know the directions. To have feed-back is crucial.
One evaluating tool we will use is the Team Performance Observation Tool (TPOT) from TeamSTEPPS (Team Strategies and Tools to Enhance Performance and Patient Safety). It is “an evidence-based set of teamwork tools, aimed at optimizing patient outcomes by improving communication and teamwork skills among health care professionals.” (ahrq.gov)
They have a full training course available for institutions that we can do online, but what we are most interested is the TPOT, which will give us a really good framework to assess our team.
This year we will start to be more objective during the simulation cases and assess better our strengths and weaknesses, so we can move forward.
Be a good leader in the resuscitation room
By preparing the team appropriately (i.e. STEP-UP), using a shared mental model and closed-loop communication, you will not only be better at leading and communicating, you will do better for the patients.
After years of practice, I have concluded that it is harder than I thought to be a good leader in the resuscitation room. But it is something everyone can achieve with practice and feed-back. One of the reason is that it is so hard is that we have to leave ourselves as individuals and join a team.
Don’t just be a Tom Brady, be a Patriots.
Expanding on communication, the next post will be about debriefing and its importance after difficult or challenging cases.
Make ER Great Again. MEGA.

[…] is a document on communication to help […]
LikeLike
Good post Eric. Effective communication and a shared mental model (incl. Zero Point) are two of the cornerstones to effective teamwork and handling of difficult situations.
To be a bit of a jerk though, delegation and avoidance of task fixation are two important characteristics of the quarterback or team leader. So when your leading doctor says: “Now, I will intubate the patient” shouldn’t that task already be delegated to another team member (in the T part of the Zero Point Summary)?
LikeLike
Absolutely. This might have been influenced from my experience working as single coverage doc with little or no back-up, ending up doing things myself.
But in our reality, when part of a larger team, delegation and avoidance of task fixation are crucial like you say.
I also really like the fact that people say that there is always one team leader but it changes depending on the procedure. For example, a trauma rolls in, the team leader is classic team leader. When it comes to intubation, the leader becomes the intubator because it is the most important thing right now. All lights on him (not entirely true though, the TTL might still do other stuff like order blood, talk to the surgeons, etc). After it is completed, the lights fall back on the TTL. To me, this seems like next level but something to keep in mind.
LikeLike